Coronavirus world wide list
Содержание:
- What’s in the Covid relief bill? Democrats and Republicans in Congress claim wins
- Holiday church gathering in North Carolina leads to 97 Covid cases and counting
- High Complication Rate
- Главные мифы coronavirus
- Ok I think I’m infected, now what?
- Covid-19 cases in kids hit record high last week
- Is there a vaccine or a cure?
- Travel
- Number of cases
- Congress to vote on second Covid-19 relief package
- Handwashing
- COVID-19 by the Numbers
- Effect on the economy
- Man who fell ill on United flight from Florida died of Covid-19, coroner confirms
- Emergency Department Visits
- How do you get infected?
- Respiratory hygiene
- Spread via Droplets & Aerosols
- What if I’m sick?
- Hospital capacity
- Students thank professors in Zoom classes for ‘keeping our spirits high’ during pandemic
- What is the Coronavirus?
- Disproportionately affects the demographic
- We need to act now
What’s in the Covid relief bill? Democrats and Republicans in Congress claim wins
WASHINGTON — After more than seven months of negotiations, Republicans and Democrats in Congress are on the cusp of passing a $900 billion coronavirus relief bill and both sides are claiming victory while blaming the other for the delays in getting additional relief to Americans.
Democrats are coming away with far less than the $3.3 trillion bill House Democrats passed in May, which included nearly $1 trillion in federal funding for state and local governments. The bill set to be voted on late Monday won’t include any funding for states, a top Democratic priority. It will also exclude the Republican priority of liability protection from Covid-19-related lawsuits for businesses.
The Covid-19 relief is part of a larger government funding bill.
Both parties are touting wins that play to their constituents.
Holiday church gathering in North Carolina leads to 97 Covid cases and counting
A holiday celebration at a church in a small town in North Carolina has led to 97 Covid-19 cases as of Tuesday morning, and this number is expected to grow in the coming days, a spokesperson for the local health department told TODAY.
The gathering took place at First Baptist Church in Hendersonville, located south of Asheville, over the Dec. 5 weekend and was a multi-day event, according to a statement from the Henderson County Department of Public Health and its communications manager, Andrew Mundhenk. As of Dec. 17, the county had linked 75 cases to the event, and the health department is still working to identify close contacts of attendees.
Of the confirmed 97 cases, all are among attendees, Mundhenk said. The health department is not aware of any deaths at this time. However, «some cases» from the event have resulted in hospitalizations, Mundhenk said. The health department did not have specifics on how many.
High Complication Rate
80% of people experience mild symptoms without requiring medical attention, 15% develop serious symptoms. 5% require intensive care with specialist equipment such as ventilators. and ECMO machines.
Source: Wikipedia
We are facing global shortages of equipment in face masks and HAZMAT suits
crucial in protecting health workers. As the outbreak amplifies the number of cases, this will only become more critical.
The US has roughly 160,000 ventilators
and 264 ECMO machines
With a population of 327 million,
if 5% of patients require intensive care, this means 16.35 million people will require ventilators.
If we account for only 75% of the population becoming infected, 12.26 million people will require ventilators.
In reality not everyone will be hospitalized at the same time, if the outbreak continues over 6 months and each patient requires ventilating for 2 days, we can calculate this as follows
If 12.26 million critical patients were to be infected over a period of 183 (Six months) days,
and each case required 2 days of ventilation,
the result is 133.9 thousand ventilators required.
In reality not every ventilator will be available as many will already be occupied by patients with diseases other than COVID-19.
In order for the US to have enough ventilators, we may need to flatten the curve to span one year, in which case 67 thousand ventilators will be required per two day period
By ensuring equipment is readily available and hospital capacity is met, the mortality rate of COVID-19 can be kept as low as 1%, whereas without the necessary facilities, fatalities may swell as high as 4 or 5%
Миф 1. Передача вируса через посылки. Множество людей в нашей стране переживают за то, что новый тип вируса передается через посылки и им можно заболеть. Почтовые отправления из Китая не представляют опасности, так как в первую очередь коронавирус не может жить вне организма человека более 2-ух дней. (Конечно о такой скорости доставки aliexpress мы и мечтать не могли:) )
Миф 2. Coronavirus – это смертельный приговор. Действительно, новый тип коронавируса распространяется с высокой скоростью и считается опасным. Но статистика такова, что в более 80% случаев он протекает в легкой форме и его очень сложно отличить от обычно простуды. Смертельных случаев около 4%, в большинстве своем это очень пожилые люди и люди, которые имеют слабый иммунитет.
Миф 3. Медицинские маски не защитят вас от covid-19. В действительно маски будут довольно эффективны если рядом с вами кто-то кашляет или чихает. Всемирная организация здравоохранения рекомендует носить маски в общественных местах и менять их каждые 2-3 часа.
Симптомы COVID-19
Самыми обычными симптомами является лихорадка, сухой кашель и общая усталость (симптомы очень схожи с ОРВИ или гриппом).
Также к симптомам coronavirus относят:
- Головная боль
- Заложенность носа
- Боль в горле
- Сложность дыхания
- Озноб
- Тошнота
- Диарея
При тяжелой болезни:
- Высокая температура
- Кашель с кровью
- Почечная недостаточность
Против болезни covid-19 пока отсутствует вакцина или какое-либо специфическое противовирусное средство. В данному заболеванию у людей отсутствует иммунитет и поэтому к нему подвержены люди всех возрастом.
Эпидемия начала очень быстрое распространение, и Всемирная организация здравоохранения объявила чрезвычайную ситуацию с оценкой рисков, как очень высокие.
Основные меры профилактики COVID-19
В качестве профилактики соблюдайте основные меры:
- Значительно чаще старайтесь мыть руки
- Меньше прикасайтесь ко рту, лицу и глазам
- Отложите все поездки на территорию других стран
- Избегайте массовых скоплений людей
- Чаще проветривайте воздух в помещении и делайте влажную уборку
- Старайтесь не касаться различных предметов в общественных местах
11 февраля 2020 года заболевание получило название новой коронавирусной пневмонии — COVID-2019 (CO – это коронавирус, VI – это вирус, а D обозначает заболевание).
Ok I think I’m infected, now what?
-
Self-isolation at home has been recommended for those diagnosed with COVID-19 and those who
suspect they have been infected. -
Public health agencies have issued self-isolation instructions that include notification of
healthcare providers by phone and restricting all activities outside of the home, except for
getting medical care. -
Do not go to work, school, or public areas. Avoid using public transportation, ride-sharing,
or taxis - Those who have recently travelled to a country with widespread transmission or who have been in direct contact with someone diagnosed with COVID-19 have also been asked by some government health agencies to self-quarantine or practise social distancing for 14 days from the time of last possible exposure.
- Attempts to relieve the symptoms may include taking regular (over-the-counter) cold medications, drinking fluids, and resting. Depending on the severity, oxygen therapy, intravenous fluids, and breathing support may be required.
- The use of steroids may worsen outcomes.
Covid-19 cases in kids hit record high last week
The U.S. logged a record high number of pediatric Covid-19 cases last week, according to the American Academy of Pediatrics.
Last week alone, 182,018 new pediatric cases were reported. Since early December, cases in children have increased by 25 percent.
More than 1.8 million cases of Covid-19 had been diagnosed in children since the beginning of the pandemic. Kids represent 12.3 percent of all Covid-19 cases in the U.S., a percentage that has steadily increased in recent months.
Severe complications of Covid-19 in kids are rare, as are hospitalizations, the AAP reported. But studies have shown children can spread the virus as well as anyone else.
Death from Covid-19 is also rare among children. A total of 172 kids in the U.S. have died from Covid-19, less than 1 percent of all deaths from the disease in the U.S.
Is there a vaccine or a cure?
- No vaccine is currently available.
- Several organisations around the world are developing vaccines, using several different methods.
- By early March 2020, 30 vaccine candidates were in development, with products by Gilead Sciences and Ascletis Pharma in Phase III clinical trials.
- Several compounds, which were previously approved for treatment of other viral diseases, such as favipiravir, ribavirin, remdesivir and galidesivir, are being investigated against the coronavirus.
- Clinical trials are underway in for lopinavir/ritonavir and of remdesivir.
- Bruce Aylward, an assistant director-general of the WHO, has stated «there is only one drug right now that we think may have real efficacy and that’s remdesivir.»
Travel
Can I travel?
You can travel for urgent matters or if such travel is essential to your permitted work. Even though businesses around the state are opening up, avoid travelling long distances for vacations or pleasure as much as possible. This is to slow the spread of the coronavirus. Do not travel if you are sick, or if someone in your household has had coronavirus in the last two weeks. Do not travel with someone who is sick.
Before travelling away from your community, consider these questions from the Center for Disease Control (CDC) travel guidance:
-
Is coronavirus spreading where you are traveling?
-
Are you or those you are traveling with more likely to get very sick from coronavirus?
-
Will you be able to keep 6 feet of physical distance from others during or after your trip?
If you do travel, take steps to keep everyone safe like wearing a face covering, keeping 6 feet of physical distance from those not in your household, and washing your hands frequently.
More info: Stay home Q&A
Number of cases
Although we know the number of confirmed cases, we do not know the number of true cases.
Due to a lack of available testing kits in many countries, GP’s are discouraged from testing people exhibiting symptoms unless they also meet a specific set of criteria, thereby the current true number of people infected remains uncertain.
South Korea is testing thousands of people at a time, this could be the reason for their low fatality rate at 0.6%, they are confirming cases where people have mild symptoms, or are yet to exhibit any. In contrast to this, the US has a fatality rate of about 3.6%, where negligible testing is taking place, and perhaps only the serious cases are confirmed. The fatality rate can also be low as testing is conducted in drive-throughs, and not solely focused on patients who have been admitted to hospital.
Many countries have adopted non-pharmaceutical measures to decrease this count through means of social isolation. New Zealand and Australia have enforced for a mandatory 14 day self-isolation policy for all international arrivals. Other countries such as Singapore, Japan, and the USA have called for more lenient policies restricting travel from specific countries.
Testing is imperative to identify cases and hot zones before they develop out of control. In Seattle, where the first confirmed case was found in the US, the virus had been spreading for up to six weeks due to a lack of testing. Without testing we are blind to what we are facing, leading to suboptimal reactions.
By refusing to test as many people as possible, the number of cases can be kept artificially low, but the death rate is likely to be higher than reality.
Congress to vote on second Covid-19 relief package
Congress is expected to vote later Monday on a massive Covid-19 relief package and government funding bill, its second effort to provide direct aid to Americans struggling during the pandemic.
Congressional leaders struck a deal on nearly $900 billion in Covid-19 relief late Sunday, including a new round of direct payments and unemployment benefits for Americans, families and businesses struggling in the pandemic.
The agreement includes stimulus checks of up to $600 per person for individuals earning $75,000 per year and married couples who earned up to $150,000, with an additional $600 for each dependent under 18 living in the same household.
Handwashing
-
A number of governments advise against all non-essential travel to countries and areas
affected by the outbreak. -
There are misconceptions circulating about how to prevent infection: rinsing the nose,
gargling with mouthwash, and eating garlic are not effective. -
The CDC recommends that people wash hands often with soap and water for at least 20 seconds,
especially after going to the toilet or when hands are visibly dirty.
-
It further recommended using an alcohol-based hand sanitiser with at least 60% alcohol
by volume (or 120 proof) when soap and water are not readily available. -
The WHO also advise people to avoid touching the eyes, nose, or mouth with unwashed
hands.
COVID-19 by the Numbers
On December 21, there were 32,659 newly recorded confirmed cases. The state now has a total of 1,925,007 positive cases. There have been a total of 22,923 deaths in the state.
For county level data, access the COVID-19 Public Dashboard.
For skilled nursing facility data, visit Skilled Nursing Facilites: COVID-19.
For age group data, visit Cases and Deaths Associated with COVID-19 by Age Group in California.
Racial Demographics — A More Complete Picture
The California Department of Public Health is committed to health equity
and collecting more detailed racial and ethnic data that will provide
additional understanding for determining future action. Health outcomes are
affected by forces including structural racism, poverty and the
disproportionate prevalence of underlying conditions such as asthma and heart
disease among Latinos and African American Californians. Only by looking at the
full picture can we understand how to ensure the best outcomes for all
Californians.
The differences in health outcomes related to COVID-19 are most stark in COVID-19 deaths. We have nearly complete data on race and ethnicity for COVID-19 deaths, and we are seeing the following trends: Latinos, African Americans and Native Hawaiians and Pacific Islanders are dying at disproportionately higher levels. More males are dying from COVID-19 than females, in line with national trends.
For the additional information, visit COVID-19 Race and Ethnicity Data.
Testing in California
Twenty-five public health labs in California are testing samples for COVID-19. These labs include the California Department of Public Health’s Laboratory in Richmond, Alameda, Butte, Contra Costa, Fresno, Humboldt, Imperial, Long Beach, Los Angeles, Monterey, Napa-Solano-Yolo-Marin (located in Solano), Orange, Riverside, Sacramento, San Bernardino, San Diego, San Francisco, San Joaquin, San Luis Obispo, San Mateo, Santa Clara, Shasta, Sonoma, Tulare and Ventura County public health laboratories. The Richmond Laboratory will provide diagnostic testing within a 48-hour turnaround time. This means California public health officials will get test results sooner, so that patients will get the best care. Additional information on testing and locations to get tested in California can be found on the.
Effect on the economy
As coronavirus blazes through nations forcing businesses shut, and shopping precincts to close doors, financial markets are taking massive losses. Global economies have hit their biggest downturn since the 2008 financial crisis.
Source: Statista
Governments must select either less cases, less deaths, and a worse economy; or more cases, more deaths, and a better economy. There is a delicate balance to be met between these two variables.
We don’t know how the choices made today will play out in the long run. Judging from how virulent COVID-19 is, and with existing measures of containment falling short, perhaps it’s better to experience short term repercussions today without enforcing social isolation (As the UK has chosen), rather than experiencing negative effects to the economy for a longer duration.
China has found a resurgence of cases with citizens returning to work, suggesting that efforts to flatten the curve are an ongoing problem.
At least the planet can breathe a sigh of relief.
Source: CNN
China is seeing blue skies as industrial CO2, and NOX emissions are slashed, possibly the clearest since the 2008 Beijing Olympics.
Man who fell ill on United flight from Florida died of Covid-19, coroner confirms
Covid-19 caused the death of a traveler who fell ill aboard a flight from Florida to California last week, Louisiana authorities said Tuesday.
Jefferson Parish coroners listed «acute respiratory failure» and «Covid-19» as causes of death for Isaias Hernandez, a 69-year-old Los Angeles resident.
Hernandez had been aboard a westbound United Airlines flight from Orlando to Los Angeles last Monday. After falling ill, two fellow travelers — a nurse and EMT — performed cardiopulmonary resuscitation on him, witnesses said.
The flight was diverted to New Orleans and Hernandez died that night at a hospital in Kenner, Louisiana, according to the coroner’s report.
Emergency Department Visits
These charts show people who visited the emergency department with clinical
signs and
symptoms consistent with COVID-19 illness (including flu-like illnesses and
pneumonia) during the past three months, and those who were then admitted to the
hospital. While some of these people did not have a positive molecular or
antigen test, these charts can be an
early warning sign for community
transmission of COVID-19.
Visits
Admissions
About the Data: All of the data on these
pages were collected by the NYC Health Department. Data
will
be updated daily but are preliminary and subject to change.
Reporting Lag: Our data are published with a
three-day
lag, meaning that the most recent
data in today’s update are from three days before.
This lag is due to the standard delays (up to several days) in reporting to
the
Health Department a new test,
case,
hospitalization or death. Given the delay, our counts of what has happened
in
the most recent few days are
artificially
small. We delay publishing these data until more reports have come in and
the
data are more complete.
Health Inequities in Data: Differences in health outcomes
among
racial and ethnic groups are due to long-term structural racism, not
biological
or personal traits.
Structural racism — centuries of racist policies and discriminatory
practices across institutions, including government agencies, and society
— prevents communities of color from accessing vital resources (such
as
health care, housing and food) and opportunities (such as employment and
education), and negatively affects overall health and well-being. The
disproportionate impact of COVID-19 on New Yorkers of color highlights how
these
inequities negatively influence health outcomes.
Review
how we are working to address inequities during this public health
emergency (PDF).
How do you get infected?
- The main route of transmission is respiratory droplets and close contact.
- When you sneeze or cough, you send out droplets of fluid from your nose and mouth.
-
Those droplets can carry infections, and when they enter someone else’s enter the eyes, nose
or mouth, the infection can make them sick. This is the way the flu and many viruses are
spread. - Most often, you need to be close to the person (within 6 feet) for it to spread this way.
-
There is the possibility of aerosol transmission when exposed to high concentration aerosol
for a long time in a relatively closed environment. -
The WHO has stated that the risk of spread from someone without symptoms is «very low» and
that fecal transmission is «low».
Respiratory hygiene
-
Health organizations recommended that people cover their mouth and nose with a tissue when
coughing or sneezing (which should then be disposed of immediately), or with a sleeve if a
tissue is not available. -
The use of surgical masks by those who may be infected has also been recommended, as they
can limit the volume and travel distance of expiratory droplets dispersed when talking,
sneezing, and coughing. -
There is no evidence to show that the wearing of surgical masks by uninfected people at low
risk is effective. -
Only China has specifically recommended the use of masks by healthy members of the public,
while face masks have been widely used by healthy people in Hong Kong, Japan, Malaysia, and
Singapore.
Spread via Droplets & Aerosols
After an infected person coughs, droplets can travel 1.5 meters away. The droplets can then persist on a surface for up to nine days, varying with temperature & humidity.
This type of contagion can be especially prevalent in healthcare settings
Due to the risk of aerosol transmission, China & South Korea have been actively spraying disinfectant in streets and subways shared by the public at large.
In the cruise ship harbored off the coast of Japan, Diamond Princess, the case count continued to increase despite stringent social isolation measures and a quarantine lockdown. This suggested that COVID-19 had possibly passed through air ducts into separate cabins.
What if I’m sick?
What are the symptoms of COVID-19?
Typically, human coronaviruses cause mild-to-moderate respiratory illness. Symptoms are wide ranging and can be similar to the flu, including:
-
-
Fever
-
Cough
-
Shortness of breath
-
Chills
-
Repeated shaking with chills
-
Muscle pain
-
Headache
-
Sore Throat
-
New loss of taste or smell
-
COVID-19 can cause more severe respiratory illness. If you have any of the emergency warning signs listed below, you should contact your medical provider immediately:
-
Trouble breathing
-
Persistent pain or pressure in the chest
-
New confusion
-
Bluish lips or face
What if I have symptoms?
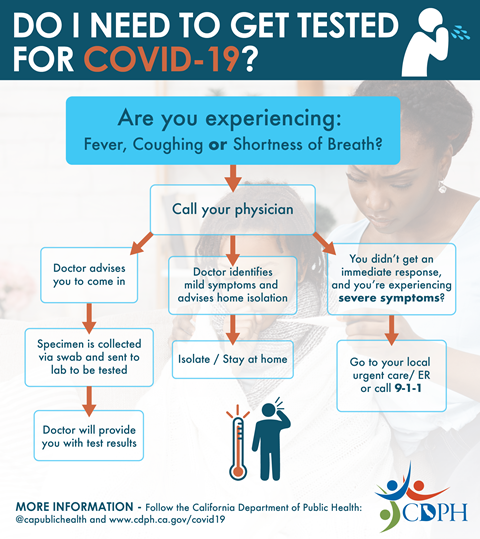
Patient: If a person develops symptoms of COVID-19, including fever, cough or shortness of breath, and has reason to believe they may have been exposed, they should call their health care provider before seeking care. Contacting them in advance will make sure that people can get the care they need without putting others at risk. Please be sure to tell your health care provider about your travel history. You can also take the following precautionary measures: avoid contact with sick individuals, wash hands often with soap and warm water for at least 20 seconds.
Health Care Provider: Patients who may have infection with this novel coronavirus should wear a surgical mask and be placed in an airborne infection isolation room. If an airborne infection isolation room is not available, the patient should be placed in a private room with the door closed. Health care providers should use standard, contact and airborne precautions and use eye protection. Please see «Update and Interim Guidance on Outbreak of 2019 Novel Coronavirus (2019-nCoV) in Wuhan, China» for more information about infection control. The Public Health Department will issue All Facility Letters to regulated healthcare facilities within California with updated information and guidance; these can be found on the AFL webpage.
What should you do if you think you’re sick?
Call ahead: If you are experiencing symptoms of COVID-19 and may have had contact with a person with COVID-19, or recently traveled to countries with apparent community spread, call your health care provider before seeking medical care so that appropriate precautions can be taken.
Hospital capacity
COVID-19 patients in critical condition require labour intensive medical attention and respiratory devices. They also tend to be hospitalized for multiple weeks, pushing available medical resources to limits.
We need to flatten the curve to maintain an active case count below hospital capacity. This creates even distribution to hospital resources to keep mortality rates low with the same number of people affected.
Source CDC
The curve can be flattened through non pharmaceutical interventions such as social distancing and proactive testing which slow the outbreak to manageable levels.
Students thank professors in Zoom classes for ‘keeping our spirits high’ during pandemic
Students from The College of New Jersey, York University, and Chapman University surprised their professors during Zoom classes to thank them for their work during a challenging year.
Prof. Mario Di Paolantonio of York University in Toronto, where he’s been an educator for over 20 years, spent time reworking his in-person coursework for online learning due to the pandemic and found this surprise by his Educational Studies students to be «a real gift.»
«I think there was this feeling of thanks, not just to me, but for the whole thing that we managed to do, that we we did something educational, in spite of it all,» Di Paolantonio, 55, told NBC News. «Very difficult conditions, you know, with people being in their own homes, with some having childcare issues as well, and other things…but they committed they got through it, we got through it.»
Kaitlyn Gong, a student at Chapman University in Southern California — taking classes remotely from Oakland — said learning virtually was «not easy at all» for her first semester. She credits Prof. James Brown for pushing her to succeed and was among the students who surprised him over his Zoom class to thank him. «And he’s done such a great job at keeping our spirits high,» Gong, 18, told NBC News
«Sometimes when you get to the end of the semester, and you give your last lecture, students will stand up and applaud or something like that,» Brown, 71, told NBC News. «That’s very moving too, but this is, you know, it’s a different format for some who’ve been teaching in this format. And so holding up the signs, yeah, was unique.»
-
2019 Novel Coronavirus (2019-nCoV) is a virus (more specifically, a coronavirus)
identified as the cause of an outbreak of respiratory illness first detected in Wuhan,
China. -
Early on, many of the patients in the outbreak in Wuhan, China reportedly had some link
to a large seafood and animal market, suggesting animal-to-person spread. -
However, a growing number of patients reportedly have not had exposure to animal
markets, indicating person-to-person spread is occurring. -
The name coronavirus is derived from the Latin corona, meaning «crown» or «halo», which
refers to the characteristic appearance reminiscent of a crown.
Disproportionately affects the demographic
People who are 60+ are most at risk, with the most fatalities occurring in those 80+. Gender differences do not appear to be significant.
Looking into data from South Korea, in total there were more confirmed cases in females, but fatalities are almost twice as high in men.
The larger number of female cases can be attributed to healthcare roles traditionally housing more women, and higher fatalities in men to more smoking tendencies. However, the sample size is too small to draw conclusive results.
Kids seem to be spared from the virus.
Source: Midas Network
The immune system naturally weakens with age, COVID-19 can be fatal when combined with pre-existing medical conditions. We need to protect the elderly around us by setting up systems to let them live in isolated areas where they are able to support themselves.
We need to act now
Wuhan China, where COVID-19 originated and hit the hardest in China, went into lockdown on January 22nd, 2020. Following this, the number of confirmed cases continued to increase until February 4th, almost two weeks later when the number of new cases finally dropped.
Source Wikipedia
Any action taken today is felt about two weeks later, and patients may only be discharged from hospitals up to a month later. When Wuhan went into Lockdown they had 15,000 cases, yet they peaked two weeks later at after cases reached 80,000. Italy went into lockdown on March 9th, when they had 9000 cases, today their count continues to increase. When the response to our actions is delayed it makes it hard to measure how much effect they have had.
We can only estimate the number of true cases. Although a country reports a certain number of cases, in reality there may be ten times more due to the slow onset of COVID-19.
From looking at countries that went into lockdown, China, South Korea, and Italy, the number of confirmed cases continues to increase for two weeks before progression is abated.
The number of true cases are likely to be an order of magnitude higher than the real case count.
The virus transmission grows exponentially, humans generally understand linear change, but have a hard time understanding exponential change. Although only a small number of the population are infected,
the current doubling time is around 3 to 4 days. Cases double every 3 to 4 days.
Within three weeks of the virus infecting 1% of the population, it can double 6 times to infect 64% of the population.






